|
Recently, discussions have emerged on television, in magazines, on the radio, or by word of mouth highlighting the phrases “Low T” or “Andropause;” But what do these phrases mean? As men age, they begin to experience symptoms that fall in line with hormonal imbalance, particularly low testosterone1 Many men never seek treatment and go about their daily lives experiencing significant decline in testosterone production, resulting in symptoms like fatigue, low libido, decreased strength, decreased mental capacity, anxiety, depression, decreased lean body mass, fatigue, and decrease in bone mineral density, among others.2 As awareness of this diagnosis grows, more men are seeking treatment and finding ways to travel through the years without feeling the emotional and physical changes that tend to come with age. One of the main offerings to help solve this is the obvious – using agents to replace testosterone.
WHAT DOES TESTOSTERONE REPLACEMENT TREATMENT LOOK LIKE?When practitioners discuss the topic of testosterone treatment with their patients, they talk about replacing it with agents such as gels, creams, and injections or they attempt to encourage a more natural boost to a man’s testosterone by using herbs and nutraceuticals. While these methods are undoubtedly an approach towards addressing the symptoms, these methods do not address the underlying cause of the testosterone deficiency. To really get to the root of the issue, we need to also look at the individual’s diet, lifestyle, stress level, and their overall health. In this article, we will discuss the basics: key areas that influence testosterone production and the interrelated players in the male sex hormone system. Treatment for each of these areas may include a natural, bioidentical, or pharmaceutical method resulting in alteration of the entire system. THE MALE SEX HORMONE CYCLEThe male sex hormone cycle is incredibly complex and is involved in many processes in the body. If we start in the brain, the simplified sex hormone cycle may look something like this:
ADDITIONAL OPTIONS FOR TESTOSTERONE TREATMENTIt’s apparent that hormones are comprised of a series of complex systems. Thus, they can be adjusted at many different steps in the hormone cycle. Let’s look at a few alternatives:
This overview is To Be Continued, looking into each area and how it can be impacted, by diet, exercise, supplements, bioidentical hormones and pharmaceuticals. REFERENCES:
0 Comments
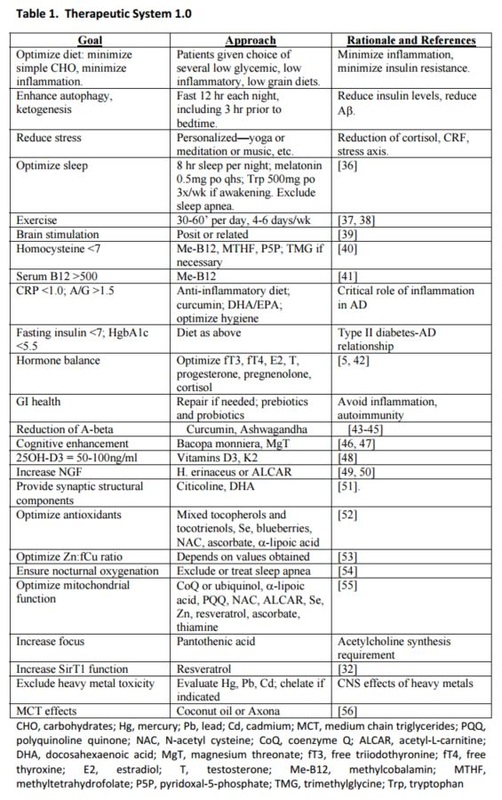
Studied Naturopathic approaches towards cognitive impairment, memory loss, and Alzheimer’s.I have encountered a number of patients requesting more information recently about what they can do to preserve their memory as they age. There are many books available with attendant products, gadgets, and techniques to improve and preserve memory. While some methods may not be entirely effective, there are many that have a proven history. All that said, there haven’t been any studies that I’ve come across that have looked at the multitudes of potential causes of cognitive decline and sought to address and treat these potential causes in a comprehensive manner. However, a recent series of personalized case studies out of UCLA published last year does in fact aim to identify potential causes and treatment of memory decline. It’s so well customized according to the various risk factors, that the structure and plans could have originated from Dr. Abercrombie or myself! This is exciting stuff! While I may tune some of the components or metrics, the study acts as a great starting point for anyone looking to assess a number of possible influences towards cognitive decline and to target specific treatments towards them. The study is provides both the framework for testing and assessments, as well as concepts for treatment. One aspect about of the study that sets it apart from many others, is the emphasis on mitochondrial, methylation and hormone function; areas that are frequently not accounted for. When implementing this treatment for a patient, I also pay close attention to the hypothalamic-pituitary-adrenal axis, thyroid function, and the remainder of the genetically-related methylation pathway, as these can frequently be ‘upstream’ influencers on the metrics that are directly monitored in the study. As the study notes, when you’re dealing with 36 different possible avenues, there may very well be 20+ interventions, thus making it difficult to initially implement. My suggestion is to complete proper laboratory work, exams, and conduct a lifestyle assessment to identify the areas that need improvement, then to prioritize focus on treating one section at a time The table below from the study lists key metrics on the left, and a few possible treatments in the middle. Keep in mind that this is just a single example and that it is absolutely not a direct template that should be followed, given that each example is customized to the individual. (http://www.impactaging.com/papers/v6/n9/full/100690.html)
The study outlines the treatment protocols for several individuals, with similar stories to those I have seen in my office. In one example, through the course of treatment, a 67yo woman with a family history of cognitive decline and a personal 2-year history of worsening memory participated in the customized treatment. After 3 months of implementation of the personalized treatment plan, she noted a reduction or complete elimination of ALL of her initial concerns. What is an example of the Cognitive Treatment Plan? This patient’s particular plan involved: (1) eliminate all simple carbohydrates, leading to a weight loss of 20 pounds (2) eliminate gluten and processed food from the patient’s diet, with increased vegetables, fruits, and non-farmed fish (3) to reduce stress, the patient implemented a regular yoga practice (4) as a second measure to reduce job stress, meditation was implemented for 20 minutes, twice per day (5) body appropriate dose of melatonin each night (6) she increased her sleep from 4-5 hours per night to 7-8 hours per night (7) body appropriate dose of methylcobalamin (B12) each day (8) body appropriate dose of vitamin D3 each day (9) body appropriate dose of fish oil each day (10) body appropriate dose of CoQ10 each day (11) optimized oral hygiene using an electric flosser and electric toothbrush (12) following a discussion with her the patient’s primary care provider, she reinstated a hormone replacement therapy program was reinstated that had previously been discontinued (13) a minimum of 12 hour fasting between dinner and breakfast, and for a minimum of three hours between dinner and bedtime (14) Regular exercise for a minimum of 30 minutes, 4-6 days per week. I’m excited about this matrix approach towards treating cognitive and memory decline and look forward to seeing further studies emerging from this group. In the meantime, we will be using this research study as a starting point, further customizing it with extra Naturopathic related research and treatments and beginning similar treatments on a larger scale in 2016. If you’d like to participate, please do drop the office a line. The study may be found at http://www.impactaging.com/papers/v6/n9/pdf/100690.pdf and a similar summary article athttp://neurosciencenews.com/alzheimers-memory-loss-reversal-1377/ Estrogen decrease over our lifetime is a natural process of aging as we approach peri-menopause and enter menopause. Although a natural process, decreasing levels of estrogen can have less than desirable side effects, most importantly its effects on cardiovascular disease. Low estrogen in menopause leads to:
What is Bio-identical Hormone Replacement Therapy?Bioidentical hormones are made from natural soy or yam components that are synthesized to be identical to the hormones that are made in your body. Bioidentical hormone therapy is specifically created by a compounding pharmacy for your individual needs determined from thorough hormone testing. Proper estrogen and progesterone ratios can then be reestablished as well as uncovering testosterone, cortisol, and DHEA imbalances. Bioidentical hormones are used together with naturopathic therapeutics, exercise and nutritional therapies to increase health and vitality. Who Needs BHRT?Pre-menopause:Pre-menopausal women that are regularly cycling may have symptoms indicating hormone imbalance. Symptoms may include: · PMS(mood changes, acne, breast tenderness, painful cycles and irregular menses) · Migraines · Fatigue · Anxiety · Miscarriage/Infertility Peri-menopause:Peri-menopausal woman will start to have changes in their menstrual cycle commonly skipping monthly cycles as the hormone levels start to decrease. Women with chronic illness, depletion, adrenal fatigue and long term use of oral contraceptives tend to notice peri-menopausal changes earlier than other women. The average woman enters perimenopause at 45 years old. Symptoms may include those above as well as:
· Cardiovascular disease · Osteopenia/osteoporosis · Collagen changes and increased infection Naturopathic Treatment Plan and Assessment includes:
So, a few folks have recently asked me the difference between an allergy sensitivity and a sensitivity. Here is a personal case in point:
When I eat pecans, my tongue tingles and my eyes water a little. When I eat a brazil nut, my lips swell and my throat closes. In mid-June, I'm sneezing and having watering eyes non-stop. These are all ALLERGIES, where your immune system is directly and immediately attacking the substance and you have an allergic response. On the other hand, SENSITIVITIES are far more subtle. Last night, I thought that I'd try soy for the first time in a year or two, in the form of soy mayonnaise in a lovely potato salad. After 2 hours, I just became a little chilly. After 3 hours, I was just a little grumpy. I didn't really notice the change objectively, only in retrospect. This morning, I feel what might only be described as 'hung-over', although I haven't had any alcohol in a while. Other people might get a little bloated, gassy, spacy, brain-fogged, etc. Others might develop some unexplained skin rash or itching. The feelings might happen within hours, or might take a couple of days to appear. As a side note, the symptoms might also take days to clear, which can make it hard to pinpoint the source. These are pretty vague, right? Hard to spot, hard to identify. Food sensitivities are a bear to identify and take fortitude to try to eradicate. The distinction between sensitivities and INTOLERANCES is less distinct. It almost seems that it's a bit of a continuum, where intolerance leans towards the more immediately physically frustrating end. The prime example of this is lactose intolerance - a person drinks milk and within an hour or two, they're gurgling, burping and having abdominal pain and perhaps diarrhea. This is due to their digestive system not having the ability to break lactose down into the things that your body can absorb. Lactose stays in the gut and starts to act like milk of magnesia, or your other favorite laxative of that type. Intolerances are often due to the body not having the ability to convert a substance into something that it can deal with. "So, you may be asking, "I've got some of the things you talked about, how do I know which allergy type I have for sure?" Well, like most things in medicine, "that depends". Allergies can usually be detected via a blood test or skin scratch test, especially if you've been exposed to the substance somewhat recently. Intolerances may be detectable by looking for specific elements in urine or stool, or may not be easily detectable. Those more subtle intolerances and food sensitivities can only reliably be determined by fully removing the item from your body for a period of time and then 'challenging' it by trying it again and seeing if the symptoms return. I should note that some sensitivities may show up in specialized blood tests or via other alternative methods, but the removal/challenge test is the reliable gold standard, albeit the one that is more irritating to try. This isn't a full breakdown nor analysis of the topic, just something that I thought that I would share based on my own experience from last night. If you'd like to learn more, or would like help digging into your own concerns, feel free to drop me a line. Dr Adam Sandford, NMD For all the folks that say that a medical treatment is bunk until it has a massive body of evidence behind it: Remember that any research that is ever done, is done with the prior assumption or knowledge that what they're testing IS potentially, likely or empirically, effective.
Things just don't magically 'start working' after a good study is published. This is where logic flaws occur, Chicken/Egg style. So, for those that are able to extrapolate from what is known effective (research or clinical), to what should be effective, I applaud you. This is where you see the distinction between the slowly dying concept that only the double-blind randomized controlled study is valid, and the new concepts of "Evidence Based Medicine" and, even more extrapolatory'y, "Evidence Informed Medicine", come about. If you want to move the paradigm, get new treatments accepted into the mainstream, you need to take those cautious, brave, steps ahead. These thoughts stem from an article that I read a year or so ago... It says that there is finally some research that might indicate why acupuncture works. After clear clinical results for 2000+ years in China and 40+ years in the US. Why have studies been done? Because the medicine has been practiced, and shown effective, time and again. So - do you have a modality that works? Get the case-studies together, find research partners, drive it home. We practitioners of natural medicine might feel encroached upon, as MDs, NPs & DOs pick up some of our methods.... but really, that's just our egos (and pocket-book-based fears). The truth is, keeping it to ourselves only hurts the patient. Which is the opposite of Primum Non Nocere. http://www.examiner.com/holistic-science-spirit-in-national/new-scientific-breakthrough-proves-why-acupuncture-works Dr Adam Sandford, NMD |
Adam SandfordWhere Nature Meets Science Archives
February 2016
Categories |
 RSS Feed
RSS Feed
